Question 13#
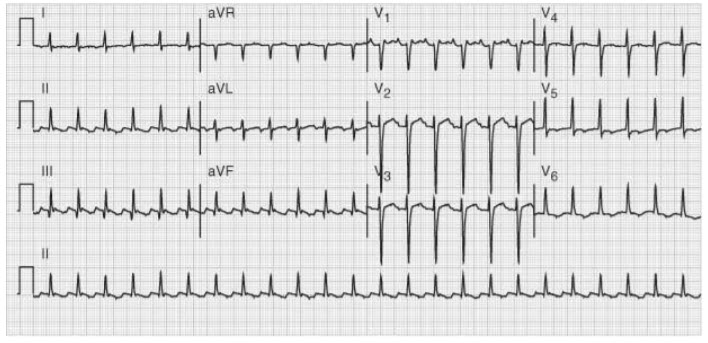
You have been following a 72-year-old man admitted to the hospital with pneumonia. On the third day of his hospitalization you are called to the bedside by the nurse because of a heart rate of 150 beats/minute. The nurse has already printed an EKG (see below). The patient’s current blood pressure is 118/89. He reports feeling weak and appears anxious but denies chest pain and does not appear to be confused or drowsy.
What is the next best step in management of this patient?
A. Administer IV beta-blocker such as metoprololB. Administer IV dihydropyridine calcium-channel blocker such as nicardipine
C. Arrange emergent electrical cardioversion
D. Order STAT cardiac biomarkers including troponin levels
E. Begin therapeutic IV heparin
Correct Answer is A
Comment:
The patient has developed atrial flutter with a 2:1 conduction. Although supraventricular tachycardia (SVT) or ventricular tachycardia (VT) may occasionally present with a rate of 150/minute, the most common cause of that particular heart rate in an elderly hospitalized patient is A-flutter. The saw tooth pattern on the telemetry strip represents the circuitous atrial depolarization at an atrial rate of 300. Atrial fibrillation/flutter is more likely to develop in predisposed individuals when exposed to physiologic stress. Once atrial flutter or atrial fibrillation with rapid ventricular response has been diagnosed, the rate needs to be controlled. Although the patient has not yet decompensated, it is unlikely that an elderly heart will be able to maintain a rate of 150 for an extended period of time. Carotid massage, ocular pressure, or Valsalva maneuvers can be attempted to slow the heart rate, but medications are usually required. The first-line agents are AV nodal-blocking agents such as beta-blockers and non-dihydropyridine calcium-channel blockers (such as diltiazem). If patients do not respond to rate control, antiarrhythmic agents such as amiodarone can be employed. Dihydropyridine calcium-channel blockers (answer b) may have a greater effect on blood pressure than heart rate, leading to hypotension. Immediate electrical cardioversion (answer c) is the treatment of choice for a patient with hypotension or evidence of end-organ hypoperfusion (confusion, chest pain, oliguria). Our patient, however, does not appear to have decompensated yet. Checking for lab evidence of myocardial ischemia (answer d) is unlikely to be helpful at this time. Even if the patient has underlying coronary artery disease, elevated biochemical markers will not change the immediate management, that is, control of the ventricular rate. The patient may very well need to be anticoagulated (answer e) depending on the need for cardioversion and risk of cardioembolism (as derived from the CHADS2 score), but this will not take precedence over immediate rate control to decrease myocardial oxygen demand.