Question 4#
A 58-year-old man with congestive heart failure (CHF), hypertension, and dyslipidemia presents to his physician with low back pain. He complains that he was lifting a heavy box 1 week ago and felt sudden pain in his lower back. He denies any incontinence, lower-extremity weakness, or paresthesia. He has been taking acetaminophen and naproxen around the clock with little effect. His chronic medications include aspirin, carvedilol, furosemide, losartan, simvastatin, and niacin. There is some tenderness to palpation of the paraspinal muscles along the lower back, but the rest of the musculoskeletal and neurologic examinations are normal. Laboratory values are significant for a potassium of 5.2 mEq/L, a BUN of 42 mg/dL, and a creatinine of 1.9 mg/ dL (baseline 1.2 mg/dL). A urinalysis is unremarkable except for few hyaline casts.
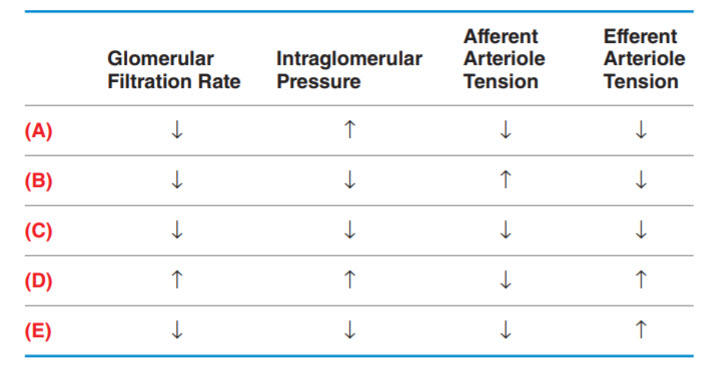
Which of the following best represents the physiologic changes in the kidney that led to this patient’s acute kidney injury? (Note: GFR is glomerular filtration rate, IGP is intraglomerular pressure, AAT is afferent arteriole tension, and EAT is efferent arteriole tension.)
B. (B)
C. (C)
D. (D)
E. (E)
Correct Answer is B
Comment:
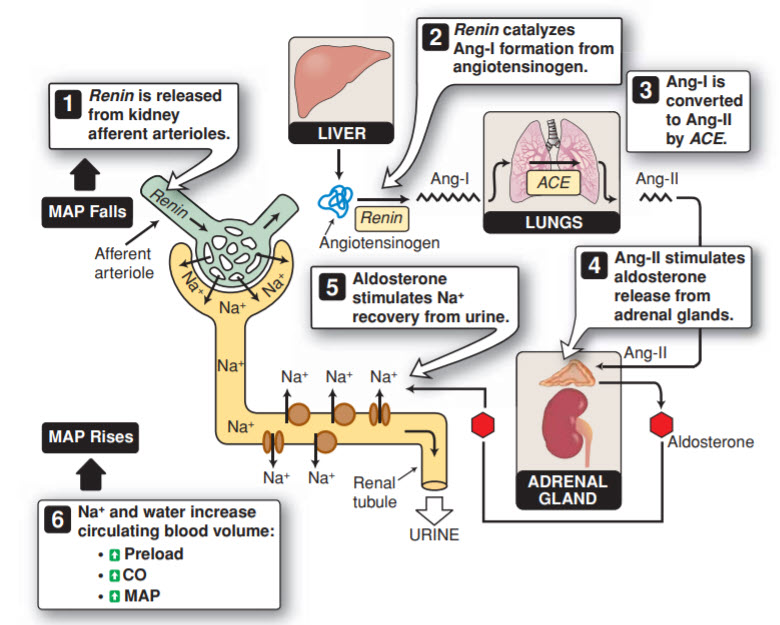
Decreased GFR, Decreased IGP, Increased AAT, Decreased EAT. This patient has prerenal AKI as indicated by the abrupt rise in creatinine, the BUN to creatinine ratio >20, and a bland urinalysis with few hyaline casts (nonspecific, but can be found in prerenal AKI). It is important to recognize risk factors for AKI, and this patient has a few. He has a baseline decrease in effective circulating volume due to heart failure, which causes two important results. The first is an increase in sympathetic activity and therefore an increase in systemic vascular resistance. An increase in norepinephrine causes afferent arteriole vasoconstriction, decreasing the GFR. The second important result of decreased effective circulating volume is activation of the renin–angiotensin–aldosterone system (RAAS, Figure below) by the kidneys in response to decreased blood flow. Angiotensin II causes efferent arteriole vasoconstriction, increasing the GFR. Overall, the net effect of decreased effective circulating volume is a decrease in GFR, which will continue to decline as activation of the RAAS leads to salt and water retention that worsens the patient’s already reduced cardiac function. However, the patient is on appropriate medications to counteract some of these harmful responses: diuretics, a β-blocker, and an angiotensin receptor blocker (ARB).
Another important consideration in this case is the patient’s use of both an ARB and an NSAID. ARBs will block the effect of angiotensin II on the efferent arteriole, thus causing relaxation of the efferent arteriole (decreasing IGP and GFR). The kidneys produce prostaglandins (primarily prostaglandins E2 and I2) that cause afferent arteriole vasodilation to preserve renal blood flow, and prostaglandin synthesis is elevated in situations of decreased effective circulating volume. By blocking the cyclooxygenase (COX) enzymes, NSAIDs inhibit the production of these prostaglandins, which leads to afferent arteriole vasoconstriction (decreasing GFR). It is important to remember that the combination of ACE inhibitors or ARBs with NSAIDs can lead to prerenal AKI or ischemia-induced ATN. (Note: Ang-I is angiotensin I, Ang-II is angiotensin II, CO is cardiac output, and MAP is mean arterial pressure.)