Question 7#
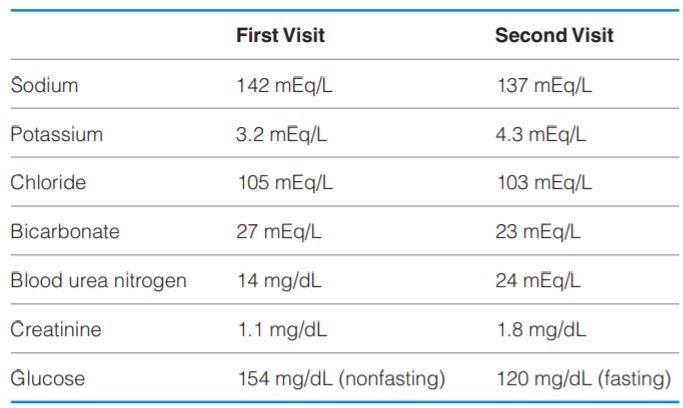
A 52-year-old man presents for a routine physical examination. He has not been to a primary care physician since he was a teenager, and now he wants a colonoscopy since his friend was recently diagnosed with colon cancer. He denies any medical history and takes no medications. He is found to be hypertensive during his clinic appointment (164/98 mmHg), and the diagnosis of hypertension is later confirmed with the use of outpatient blood pressure monitoring. On examination, a bruit is heard over the left carotid artery, an S4 is heard on cardiac auscultation, and he has weak lower-extremity pulses. He has baseline laboratory tests drawn, is started on lisinopril, and is instructed to follow up for repeat laboratory work 1 week later. At the follow-up appointment, his blood pressure is 172/102 mmHg and the following laboratory results are seen.
What should be done next in the management of this patient?
A. Add hydrochlorothiazideB. Add metformin
C. Stop lisinopril
D. Continue the current management and repeat laboratory tests in 2 weeks
Correct Answer is C
Comment:
Stop lisinopril. This patient has an abrupt rise in creatinine after 1 week of taking an ACE inhibitor, indicating that this medication may have caused acute renal failure. One potential side effect of ACE inhibitors and ARBs is a reduction in GFR, which occurs within several days after starting therapy. Although it is rare for these medications to cause AKI, patients with the following conditions are at risk: chronic kidney disease (CKD), polycystic kidney disease, heart failure, hypertensive nephrosclerosis, and bilateral renal artery stenosis.
This patient has hypertension with physical examination findings that suggest chronic hypertension (S4) and peripheral arterial disease (carotid bruit, weak peripheral pulses). In addition, he has hypokalemia at baseline. One condition that should be considered is bilateral renal artery stenosis from atherosclerosis. Because patients with this condition have poor kidney perfusion at baseline, they are in a high renin, high aldosterone state (potentially causing hypokalemia) with dilation of the afferent arteriole and vasoconstriction of the efferent arteriole to maintain GFR. ACE inhibitors cause relaxation of the efferent arteriole through a reduction in angiotensin II, further decreasing GFR and potentially causing ischemic AKI. Other clues to the diagnosis of renal artery stenosis are a renal bruit on examination and episodes of flash pulmonary edema. Bilateral renal artery stenosis can also be caused by fibromuscular dysplasia, which is less common and typically occurs in young women.
(A) The first step in the treatment of AKI is to remove the offending agent, so treating his hypertension and ignoring his AKI is not the right answer. (B) The patient is prediabetic and should be encouraged to change his diet and lifestyle before pursuing pharmacotherapy. (D) It is not appropriate to continue therapy with an agent that precipitated AKI.