Question 32#
A 19-year-old college student develops fever, headache, and nuchal rigidity. Cerebrospinal fluid (CSF) cultures grow Neisseria meningitidis. She receives appropriate treatment, and her close contacts are given prophylactic antibiotic treatment. Her mother, who took this prophylactic treatment, developed a fever and maculopapular rash afterward. She is brought to the Emergency Department, and her laboratory values are shown below.
- Sodium 133 mEq/L
- Potassium 5.4 mEq/L
- Creatinine 2.1 mg/dL (baseline 1.0 mg/dL)
- Urinalysis WBC casts and eosinophils
Which of the following represents the likely antibiotic and complication that the mother experienced?
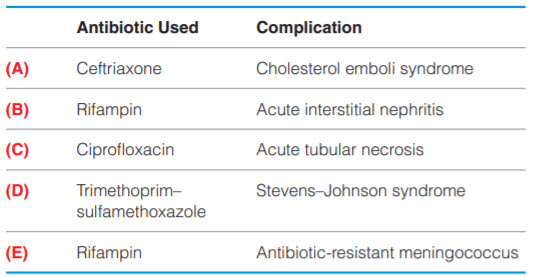
B. (B)
C. (C)
D. (D)
E. (E)
Correct Answer is B
Comment:
Rifampin, Acute interstitial nephritis. There are several recommended prophylactic drugs for close contacts of a patient with bacterial meningitis from N. meningitidis: rifampin, ciprofloxacin, and ceftriaxone. (D) Trimethoprim–sulfamethoxazole is therefore not a correct option. The next step is identifying the complication that the mother experienced. She developed an abrupt rise in creatinine (AKI) with a rash; her urine studies showed WBCs and eosinophils. Taken together, the correct diagnosis is AIN, which is a type of intrinsic renal AKI. Though it is rare to see all of these symptoms together, drug-induced AIN may produce fever, rash, arthralgias, and/or eosinophilia/eosinophiluria. It is characterized by inflammatory cell infiltrates in the renal interstitium, and the most common cause is an allergic reaction to medications. There are many antibiotics that can cause this, and all of the ones listed above can cause it. Methicillin is not used as an antibiotic anymore, but it has a very high incidence of AIN. Other etiologic medications include NSAIDs, PPIs, cimetidine, diuretics, and allopurinol.
Besides medications, other causes of AIN include infections (e.g., Legionella, cytomegalovirus, tuberculosis; pyelonephritis can cause both an acute and chronic AIN) and systemic conditions (e.g., sarcoidosis, SLE, Sjögren syndrome, IgG4-related disease, lymphoma, leukemia, and others). Withdrawal of the offending agent is the first step in managing AIN; if the patient fails to respond, renal biopsy may aid in the diagnosis and assess the extent of damage, and corticosteroids may be beneficial. The only answer choice that includes AIN is B, and rifampin is an appropriate prophylactic treatment for close contacts. (Of note, rifampin is also the prophylactic treatment of choice for close contacts of invasive H. influenzae type B infection.) (A) Urine eosinophils and rash may be seen in cholesterol emboli syndrome, but ceftriaxone does not cause this. (C) ATN would most likely show muddy brown casts on urinalysis. (E) Meningococcemia occurs with or without concurrent meningitis and often presents with a petechial rash (not maculopapular) and systemic toxicity. WBC casts and eosinophiluria suggest the diagnosis of AIN, not meningococcemia.