Question 50#
A 19-year-old young woman is referred to your office for evaluation of congestive heart failure (CHF) and MR. She has a history of complete heart block and has previously undergone pacemaker implantation. On physical examination, her heart rate is 85 bpm, respiratory rate of 16, and blood pressure 108/65 mmHg. Her jugular venous pulse is visible 6 cm above the sternal angle at 45 degrees. The point of maximum impulse is sustained but normal in location. She has a grade II/VI holosystolic murmur at the apex that radiates to the axilla. There is trivial bilateral pedal edema. A posterior– anterior and lateral chest X-ray demonstrates mild cardiomegaly. A TTE reveals moderately reduced LV systolic function with an EF of 35%. There is 2+ to 3+ posteriorly directed MR. A cardiac CT with contrast is obtained to evaluate the coronary arteries (Fig. below A and B).
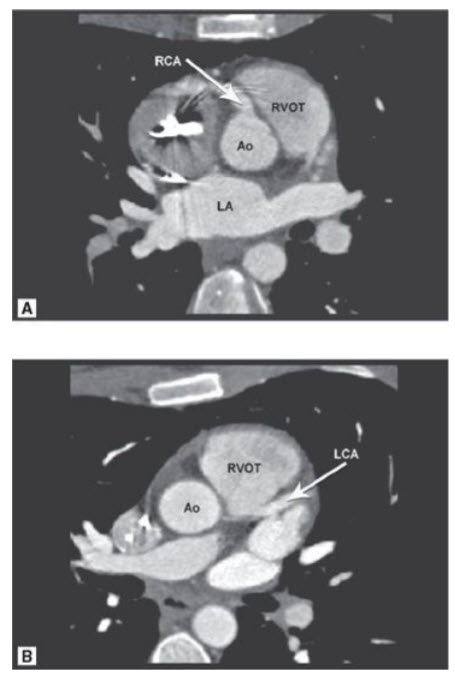
A. Double-oblique image of the aortic root at the level of the right and left sinuses of Valsalva. Ao, aorta; LA, left atrium; RCA, right coronary artery; RVOT, right ventricular outflow tract. B. Oblique axial image at the level of the left coronary artery origin. LCA, left coronary artery.
Which of the following is true regarding this patient’s condition?
A. This condition is a common cause of sudden cardiac death in athletesB. The anomaly shown represents origin of the left coronary artery from the right coronary ostium
C. Surgical reimplantation of the anomalous coronary artery is indicated
D. Patients with this condition who survive past childhood often present with varying degrees of heart failure, myocardial ischemia, and MR, depending on the development of collateral circulation
E. This condition is usually inoperable and best left alone
Correct Answer is D
Comment:
Patients with this condition who survive past childhood often present with varying degrees of heart failure, myocardial ischemia, and MR, depending on the development of collateral circulation. This CT demonstrates an anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA). Also known as Bland-White-Garland syndrome, ALCAPA is a rare but serious congenital anomaly. It is caused by either (a) abnormal septation of the conotruncus into the aorta and PA or (b) persistence of the pulmonary buds together with involution of the aortic buds that eventually form the coronary arteries. Occurrence is similar between men and women and is not considered an inheritable congenital cardiac defect. Because of the low pulmonary vascular resistance, left coronary artery flow reverses and enters the pulmonic trunk (coronary steal phenomena). As a result, the LV myocardium remains underperfused, leading to infarction of the anterolateral LV wall. This often causes anterolateral papillary muscle dysfunction and variable degrees of mitral insufficiency. Consequently, the combination of LV dysfunction and significant MV insufficiency leads to CHF symptoms (e.g., tachypnea, poor feeding, irritability, and diaphoresis) in the young infant. Collateral circulation between the right and left coronary systems eventually develops. Approximately 85% of patients present with clinical symptoms of CHF within the first 1 to 2 months of life. Left untreated, the mortality rate in the first year of life is 90% secondary to myocardial ischemia or infarction and MV insufficiency leading to CHF. In unusual cases, the clinical presentation with symptoms of myocardial ischemia may be delayed into early childhood. Rarely, a patient may stabilize following infarction and may present with MV regurgitation, periodic dyspnea, angina pectoris, syncope, or sudden death later in childhood or even adulthood, as in this patient. Treatment consists of surgical ligation of the anomalous coronary artery origin and bypass grafting to the left coronary artery. Reimplantation onto the native aortic root is typically not possible because of the friable quality of the anomalous left coronary artery ostium.