Question 3#
A 56-year-old female is admitted to the intensive care unit for management of a complete right middle cerebral artery ischemic stroke. During her stay within the intensive care unit, she has progressive somnolence over the course of 96 hours with only minor changes on her CT scan and no midline shift. Given her profound stupor, an EEG was ordered and a portion of the recording is shown in the figure below. Her current neurologic examination showed symmetric and reactive pupils at 3 mm, right gaze preference but crosses midline, profound upper motor neuron facial droop on the left, left arm and leg weakness. Patient did not follow commands or open eyes, but she continues to localize with the right arm.
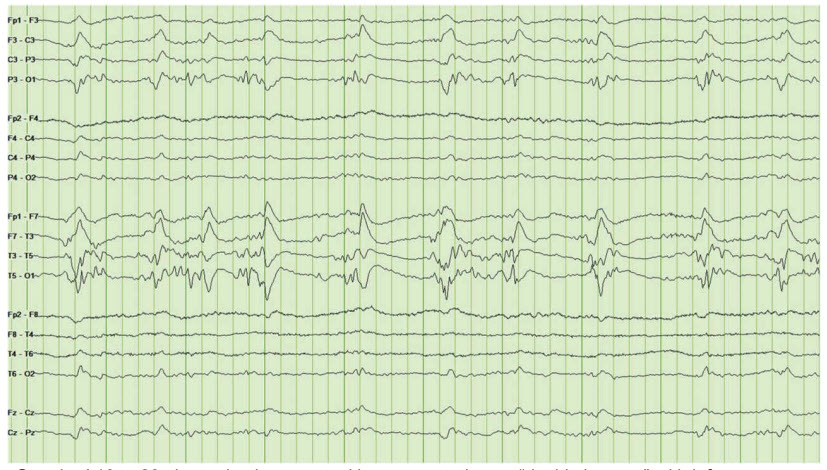
Standard 10 to 20 electrode placement with representation as “double banana” with left over right representation. There is diffuse slowing.
What is the next best step in management for this patient?
A. Continue with supportive care and no change to medicationsB. Initiation of antiepileptic medication—levetiracetam 500 mg twice a day
C. Benzodiazepine trial—lorazepam 1 mg IV once
D. Neurosurgery consultation for craniectomy
Correct Answer is A
Comment:
Correct Answer: A
Patient’s neurological examination is consistent with her right middle cerebral artery stroke. There is no clear clinical signs of seizures noted. The EEG was done to further her mental status which demonstrates spikes or sharp waves occurring at an approximately regular interval which is called periodic lateralized epileptiform discharges (PLEDs). There are no electrographic signs of seizures. The PLD nomenclature was adopted in 2012 to simplify the discussion of EEG findings within the ICU which are meant to be more descriptive while removing ambiguity from prior naming schema. PLEDs are commonly seen in patients with multiple CNS diseases such as acute ischemic stroke, tumor, infection, hemorrhage, and metabolic. In this case presentation acute stroke is the likely etiology. Given stable CT head with no signs of midline shift, there is no indication of decompressive craniectomy at this point. There are no signs of clinical or electrographic seizures, so option B and C are not indicated at this point. Continue supportive care is the right choice for now.
References:
- Hirsch LJ, LaRoche SM, Gaspard N, et al. American Clinical Neurophysiology Society’s Standardized Crticial Care EEG Terminology: 2012 version. J Clin Neurophysiol. 2013;30:1-27.
- Chu NS. Periodic lateralized epileptiform discharges with preexisting focal brain lesions. Arch Neurol. 1980;37:551-554.