Question 6#
A 60-year-old male with prior deep vein thrombosis (DVT) and pulmonary embolism (PE) on therapeutic anticoagulation, hypertension, and alcohol abuse is brought to the ED after being found down at the bottom of a flight of stairs. His GCS was 6 (eyes did not open 1, no verbal output 1, withdrawal of all extremities to painful stimulation 4). Given his poor neurologic examination, he was intubated. A head CT was completed and is shown in the image below. His initial trauma evaluation did not demonstrate any major injury, and his vital signs are normal.
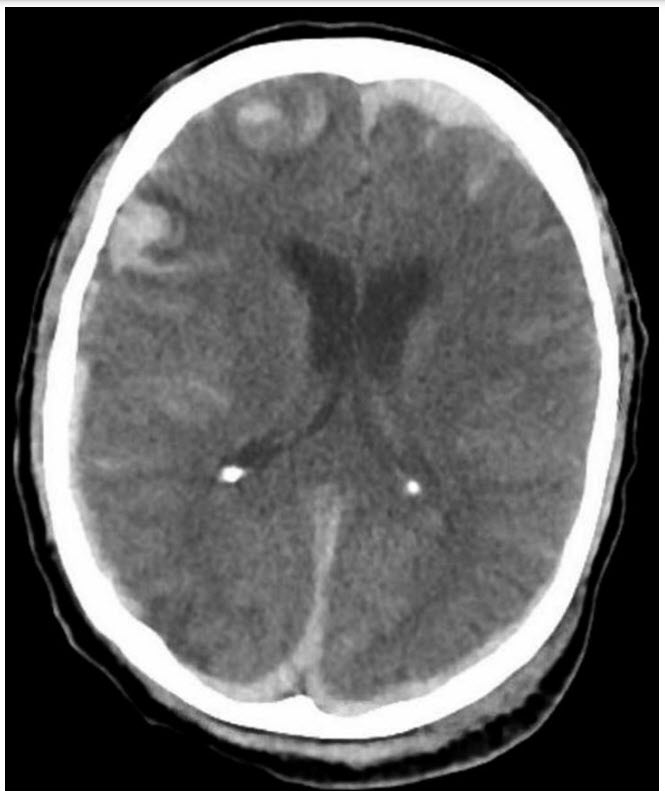
Axial noncontrast head CT. Bilateral acute subdural hemorrhage with parafalcine subdural hemorrhage. There is cortical subarachnoid hemorrhage. Bilateral right more than left frontal contusions with intraparenchymal hemorrhage.
What is the next best step in management of the patient?
A. Obtain an MRI of the brain to further evaluate the extent of TBI
B. Obtain a computed tomography angiography (CTA) head and neck for evaluation of potential intracranial aneurysm
C. Place a subdural ICP monitor
D. Start IV fluids with dextrose source
Correct Answer is C
Comment:
Correct Answer: C
ICP monitoring should be offered to patients with severe TBI (GCS 3-8) and an abnormal head CT (hematoma, contusion, swelling, herniation, or compressed basal cisterns) or severe TBI with normal head CT and two of the following: over 40 years of age, unilateral or bilateral motor posturing, or systolic BP <90 mm Hg. Although there is initial brain injury at the time of impact, there is significant risk for secondary injury including cerebral hypoperfusion and hypoxia. The goal of ICP monitoring is to limit hypoperfusion. The mainstay of management is appropriate cerebral perfusion pressure (calculated vale: mean arterial pressure − intracranial pressure), with values <50 associated with poor outcomes. ICP monitoring can be the first sign of worsening intracranial pathology. Although MRI can assist with prognosis, it is not necessary in the acute setting for ongoing initial management. MRI can be useful during the course of management to guide our outcome prognostication. Although the CT scan demonstrates SAH, it is caused by the trauma, and a CT angiogram is not needed at this time unless vascular injury (eg, carotid dissection) is suspected. Lastly, administration of dextrose prior to thiamine could precipitate Wernicke encephalopathy. Although extremely rare, and if the patient had hypoglycemia it should be treated prior to thiamine administration, there are reports of worsening neurologic symptoms in the setting of dextrose administration.
References:
- Brain Trauma Foundation. Guidelines for the management of severe traumatic brain injury. 3rd Edition. J Neurotrauma. 2017;24(S1):1-106.
- Chambers IR, Treadwell L, Mendelow AD. The cause and incidence of secondary insults in severely het-injured adults and children. Br J Neurosurg. 2000;14:424-431.
- Servadei F, Antonelli V, Giuliani G, et al. Evolving lesions in traumatic subarachnoid hemorrhage: prospect study of 110 patients with emphasis on the role of ICP monitoring. Acta Neurochir Suppl. 2002;81:81-82.
- Haghbayan H, Boutin A, Laflamme M, et al. The prognostic value of magnetic resonance imaging in moderate and severe traumatic brain injury: a systematic review and meta-analysis protocol. Cyst Rev. 2016;19:10-21.
- Charness ME, Simon RP, Greenberg DA. Ethanol and the nervous system. N Engl J Med. 1989;321:442-454.