Question 7#
A 29-year-old male was riding a motorcycle and was involved in a collision with a truck. He was placed in a cervical collar, and his GCS at the site was 7 for which he was intubated. After 3 days in the ICU, he started to move all extremities to command. An MRI of the brain is obtained, and it showed scattered foci of bleeding, as follows:
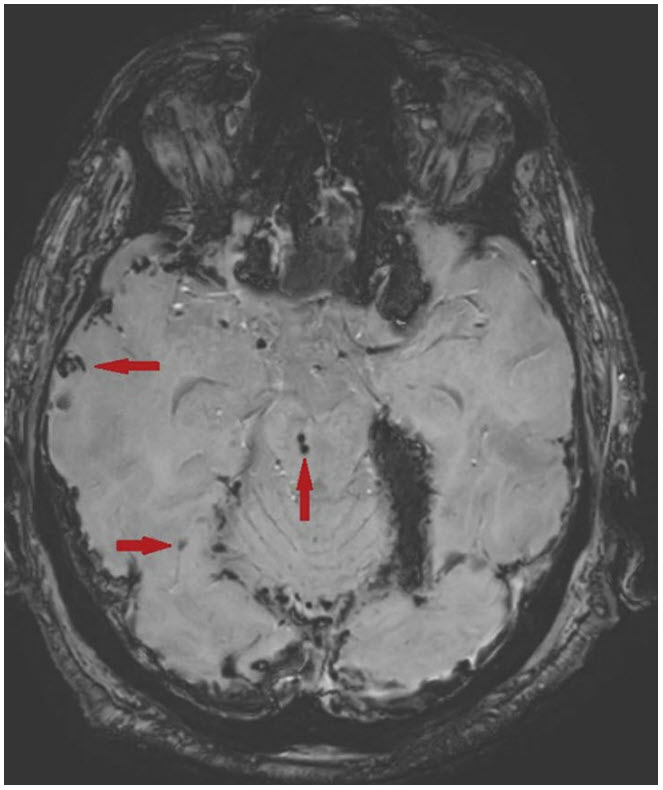
Axial susceptibility weighted imaging (SWI) on MRI. The arrows point to areas of microhemorrhages within the brain stem and temporal lobes. There is also tentorial subdural hematoma present.
Based on what is seen on the MRI, which of the following is true?
A. Immediate hemicraniectomy will reduce risk of long-term disabilityB. He is likely to return back to baseline and have no clinical deficits 30 days from admission
C. He will likely have focal seizures after 6 months from the event
D. He is likely to have cervical spinal cord injury
E. The distribution of the hemorrhagic areas is helpful in determining severity of injury
Correct Answer is E
Comment:
Correct Answer: E
This patient’s MRI brain demonstrates scattered foci of microbleeds following head trauma, which caused alterations in his mental status. This pattern is suggestive of diffuse axonal injury (DAI), which is a form of shear injury caused in the setting of abrupt rotational or torsional trauma to the head. DAI has been graded into three grades of severity, based on the distribution of the microbleeds on imaging. Grade I, if microbleeds are limited to the cortex; grade II, if they involve the corpus callosum as well; and grade III, if involving the brain stem. Overall, the higher grades are associated with more severe injury. However, recent studies suggest that we need to pay more attention to the location and proximity of microbleeds to the arousal nuclei as not all microbleeds in the brain stem carry the same prognostication value. There is no indication for hemicraniectomy in the management of isolated DAI, unless there is other evidence of increased ICP or underlying mass effect. Patients with DAI often have a prolonged ICU, hospital, and rehabilitation course. DAI outcome prognostication is challenging; it is unlikely that our patient will not have any clinical deficits in 30 days from admission. Seizures may happen after traumatic brain injuries, especially in the acute phase, but there is no evidence that DAI patients are more likely to have seizures several months after the injury. Cervical spinal cord injury can be seen in patients with traumatic brain injury, but in this case presentation, there is no clinical red flag to suggest spinal cord injury. Patient was able to move his extremities to commands.
References:
- Abu Hamdeh S, Marklund N, Lannsjö M, et al. Extended anatomical grading in diffuse axonal injury using MRI: hemorrhagic lesions in the substantia nigra and mesencephalic tegmentum indicate poor longterm outcome. J Neurotrauma. 2017;34(2), 341-352.
- Mesfin FB, Dulebohn SC. Diffuse Axonal Injury (DAI) StatPearls [Internet]: StatPearls Publishing; 2018.
- Adams JH, Doyle D, Ford I, et al. Diffuse axonal injury in head injury: definition, diagnosis and grading. Histopathology. 1989;15(1), 49-59.
- Izzy S, Mazwi NL, Martinez S, et al. Revisiting grade 3 diffuse axonal injury: not all brainstem microbleeds are prognostically equal. Neurocritical Care. 2017;27(2), 199-207.
- Meythaler JM, Peduzzi JD, Eleftheriou E, et al. Current concepts: diffuse axonal injury–associated traumatic brain injury. Arch Phys Med Rehabil. 2001;82(10), 1461-1471.