Question 1#
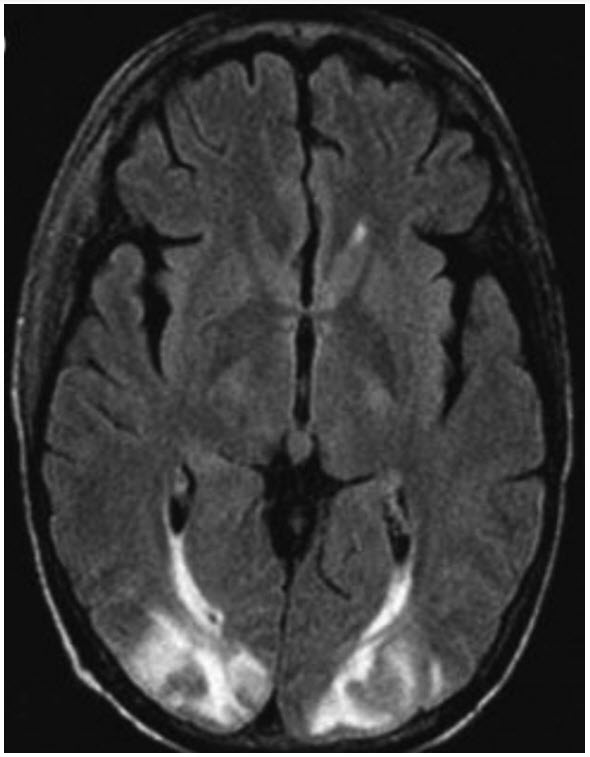
You are called to evaluate a 64-year-old man who is 3 days into his postoperative course from a heart transplant. The patient’s spouse is at bedside and describes 2 minutes of seizurelike activity, followed by persistent confusion. Vital signs are unremarkable, and a neurologic examination reveals left hemianopsia but otherwise no focal deficits. Reviews of basic laboratory studies from the day are also unremarkable. Magnetic resonance imaging (MRI) of the brain is obtained and resulted below:
Which of the following is the most likely diagnosis?
A. HypomagnesemiaB. Posterior reversible encephalopathy syndrome
C. Subarachnoid hemorrhage
D. Progressive multifocal leukoencephalopathy
E. Viral encephalitis
Correct Answer is B
Comment:
Correct Answer: B
Posterior reversible encephalopathy syndrome (PRES) is a neurological disorder that presents with a range of signs and symptoms that are reversible in nature. Nevertheless, intensive care monitoring and treatment are commonly required because of dreaded complications such as intracranial hypertension, cerebral hemorrhage, ischemia, or status epilepticus. Diagnosis is aided by the characteristic finding of vasogenic edema on neuroimaging. Frequently, this is a symmetric distribution in the parieto-occipital regions of the brain, as seen in the fluid-attenuated inversion recovery (FLAIR) sequence in the question.
PRES more commonly presents in the setting of hypertensive emergency; however, in 30% of cases, the BP is normal or only slightly elevated. Exogenic toxins can precipitate endothelial dysfunction predisposing to the syndrome. Immunosuppressive medications in the setting of solid organ transplantation and calcineurin inhibitors such as tacrolimus have been implicated in the development of PRES. Hypomagnesemia (A) is commonly seen in PRES; however, it is not likely to have precipitated this patient’s event given normal labs. Although his presentation could be consistent with subarachnoid hemorrhage (C), the MRI does not support this diagnosis. Progressive multifocal leukoencephalopathy (D) is a rare syndrome caused by the JC virus in an immunocompromised patient, where MRI may reveal diffuse areas of white matter demyelination. This would be a less likely etiology in the immediate postoperative period. Finally, viral encephalitis (E) can also produce demyelinating lesions on MRI that are localized to different areas of the brain depending on viral etiology with herpes simplex virus (HSV) classically involving the temporal lobe. However, the clinical scenario does not suggest a viral prodrome or infectious presentation.
References:
- Gao B, Lyu C, Lerner A, et al. Controversy of posterior reversible encephalopathy syndrome: what have we learnt in the last 20 years? J Neurol Neurosurg Psychiatry. 2018;89:14-20.
- Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. J Neurol. 2017;264:1608-1616.
- Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015;14(9):914-925.