Question 2#
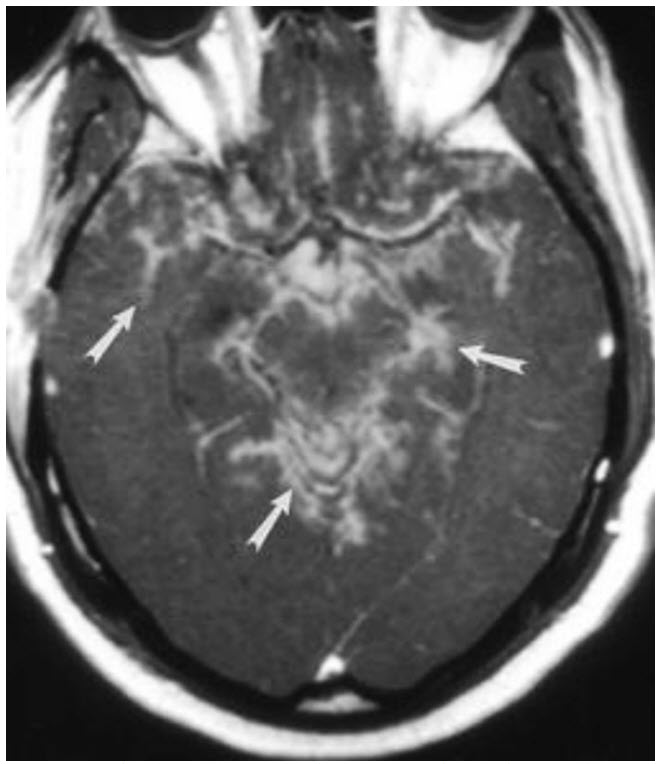
A 41-year-old African American female presents with progressive left-sided upper and lower facial muscle weakness and headaches over the last 3 months. She reports polyuria and polydipsia with >10 L of urine output per day. Lumbar puncture reveals clear cerebrospinal fluid (CSF) with WBC count 22 cells/mm3 , protein 280 mg/dL, and glucose 25 mg/dL. The gram stain and culture were negative. A slice of her MRI brain imaging showing leptomeningeal enhancement (arrows) is shown in figure below:
Which test would be MOST LIKELY to assist with the diagnosis of her condition?
A. Tensilon testB. Chest computed tomography
C. Synacthen test
D. 24-hour urinary electrolytes
Correct Answer is B
Comment:
Correct Answer: B
Sarcoidosis is a rare multisystem noncaseating granulomatous disease, which affects 3 to 10 per 100 000 among Caucasians and 35 to 80 per 100 000 among African Americans. 5% to 10% of patients with systemic sarcoidosis will have neurological involvement whereas only 17% of patients will solely present with neurosarcoidosis. Any component of the central or peripheral nervous system can be affected. Cranial mononeuropathies are common, in particular, the peripheral facial nerve is affected in 25% to 50% of neurosarcoidosis cases. Neuroendocrine dysfunction may manifest as polyuria or disturbances in temperature, libido, or appetite due to hypothalamic inflammation. Diabetes insipidus may either be central from hypopituitarism or nephrogenic from activated macrophage calcitriol causing hypercalcemia. Lung parenchyma and mediastinal lymph nodes are the most common sites affected peripherally with reported involvement in 24% to 68% of individuals presenting with neurologic sarcoidosis. The diagnosis is based on clinical symptoms, CSF evidence of inflammation (pleocytosis, elevated CSF protein), and/or MRI imaging demonstrating leptomeningeal enhancement especially around the base of the brain (arrows); however, neurosarcoidosis can involve the bone, dura mater, nerve roots, and brain parenchyma. Confirmation of systemic sarcoidosis may occur either through positive histology or two indirect indicators (gallium scan imaging, chest imaging demonstrating enlarged lymphadenopathy, or elevated angiotensin-converting enzyme [ACE] levels). Corticosteroids remain the mainstay of initial treatment followed by immunomodulatory therapy.
Chest CT scan with evidence of hilar adenopathy or parenchymal changes is consistent with sarcoidosis and may also guide a tissue biopsy diagnosis, and thus is the correct answer. Tensilon test is useful in diagnosis of myasthenia gravis and is performed by administrating edrophonium which prevents acetylcholine breakdown causing improvement in symptoms. Synacthen test (or cosyntropin test) uses adrenocorticotropin hormone (ACTH) to evaluate adrenal gland function. 24-hour urinary electrolytes may help confirm suspicion of diabetes insipidus but would not assist with the diagnosis of neurosarcoidosis.
References:
- Burns TM. Neurosarcoidosis. Arch Neurol. 2003;60(8):1166.
- Joseph FG, Scolding NJ. Neurosarcoidosis: a study of 30 new cases. J Neurol Neurosurg Psychiatry. 2009;80(3):297.
- Stuart CA, Neelon FA, Lebovitz HE. Disordered control of thirst in hypothalamic-pituitary sarcoidosis. N Engl J Med. 1980;303(19):1078.
- Smith JK, Matheus MG, Castillo M. Imaging manifestations of neurosarcoidosis. Am J Roentgenol. 2004;182:289-295.
- Pawate S, Moses H, Sriram S. Presentations and outcomes of neurosarcoidosis: a study of 54 cases. Q J Med. 2009;102:449-460.