Question 5#
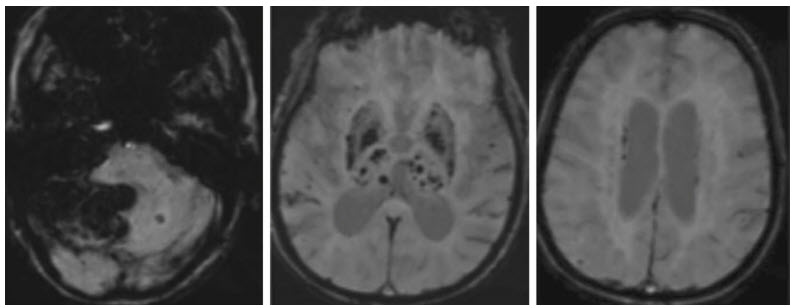
A 68-year-old female is brought to the emergency department from home for increased confusion, nausea, and emesis. She was in her usual state of health until the morning of presentation. She was last known well at 9:15 am when her husband saw her getting dressed. He heard a thud at 9:30 am and found her on the ground in the bedroom confused. EMS was called and en route she had an episode of emesis. Her initial head CT demonstrated a cerebellar hemorrhage. A follow-up MRI was completed 5 days following admission (see figures below).
What is the most likely underlying etiology of her intraparenchymal hemorrhage?
A. Cerebral amyloid angiopathyB. Hypertensive angiopathy
C. Autoimmune vasculitis
D. Infective endocarditis
Correct Answer is B
Comment:
Correct Answer: B
Given the findings on MRI, the most likely cause of her cerebellar hemorrhage is hypertension. This location is one of the common places for hypertensive bleeds (other being thalamus, basal ganglia, and pons). This is thought to be due to degeneration of the internal elastic lamina and resultant lipohyalinosis of the small vessels of the brain. The MRI of patients with hypertensive angiopathy will demonstrate areas of microhemorrhage within the same vascular regions as macrohemorrhages. Cerebral amyloid angiopathy is the most common cause of lobar intraparenchymal hemorrhage in older adults. This is the result of betaamyloid protein deposition within the intima and media of the large and medium-sized intracranial vasculature. Autoimmune vasculitis is another important etiology of intraparenchymal hemorrhage. The typical imaging finding is both ischemic and hemorrhagic infarcts of varying age. The clinical presentation of autoimmune vasculitis can mimic the presentation above, but there is typically a prodromal phase with progressive symptoms. Lastly, infective endocarditis results in intraparenchymal hemorrhage from formation of mycotic aneurysms. Infected embolic material from the affected valve will embolize and can result in formation of microhemorrhages at the sites as well as macrohemorrhages if the aneurysms rupture. Vessel imaging with CT angiography, MR angiography, or digital subtraction arteriogram are best for evaluating an aneurysm.
References:
- Campbell GJ, Roach M. Fenestration in the internal elastic lamina at bifurcations of human cerebral arteries. Stroke. 1981;12:489-496.
- Fisher CM. Pathologic Observations in hypertensive cerebral hemorrhage. J Neuropathol Exp Neurol. 1971;30:536-550.
- Tsushima Y, Aoki J, Endo K. Brain microhemorrhages detected on T2*- weighted gradient-cheo MR images. AJNR Am J Neuroradiol. 2003;24(1):88-96.
- Rosand J, Greenberg SM. Cerebral amyloid angiopathy. Neurologist. 2000;6:315-325.
- Pomper MG, Miller TJ, Stone JH, et al. CNS vasculitis in autoimmune disease: MR imaging findings and correlation with angiography. Am J Neuroradiol. 1999;20:75-85.