Question 2#
A 55-year-old male with known coronary artery disease with prior percutaneous coronary intervention of the right coronary artery 2 years prior to presentation, hyperlipidemia, and hypertension presents to the emergency department with 2 days of exertional chest pain which culminated in acute onset of “stabbing” substernal chest pain radiating to the left shoulder. Vital signs on presentation are:
- Temperature: 36.3°F
- Blood pressure: 200/89 mm Hg
- Heart rate: 81 beats per minute
- Respiratory rate: 18 per minute
- Oxygen saturation: 93% on room air
Laboratory studies are notable for a cardiac troponin-T that is undetectable.
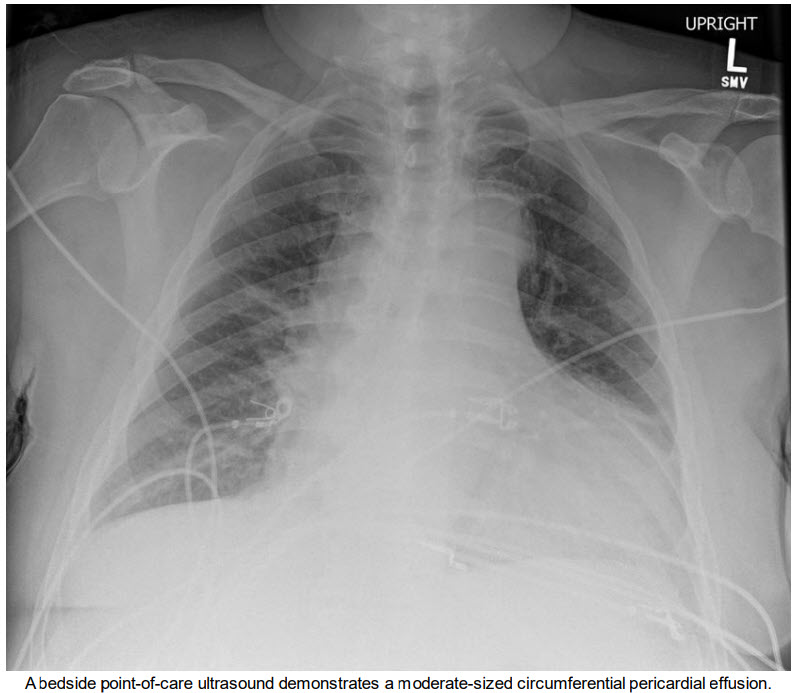
A 12-lead electrocardiogram demonstrates normal sinus rhythm, Qwaves in inferior leads, and nonspecific ST segment changes. A plain film chest radiograph is obtained (see figure below).
Which of the following is the most appropriate next step in management?
A. Coronary angiographyB. Contrasted computed tomography (CT) of the chest
C. Pericardiocentesis
D. Transesophageal echocardiography (TEE)
Correct Answer is B
Comment:
Correct Answer: B
The constellation of presenting chest pain, hypertension, widened mediastinum, and pericardial effusion must prompt a consideration of acute aortic dissection, even in the context of a presenting syndrome suspicious for unstable angina. Known risk factors for aortic dissection include male sex, history of hypertension, and advanced age, as well as connective tissue disorders. Greater than 90% of patients presenting with a type A dissection (involving the ascending aorta) report chest pain, while only 47% of patients with a type A dissection report back pain. The presenting signs for dissection include hypertension in approximately 49% of all aortic dissection presentations but only 36% of type A dissection. Plain film radiography of the chest can be suggestive but not diagnostic as only 62% of patients demonstrate a widened mediastinum.
Common complications of dissection include:
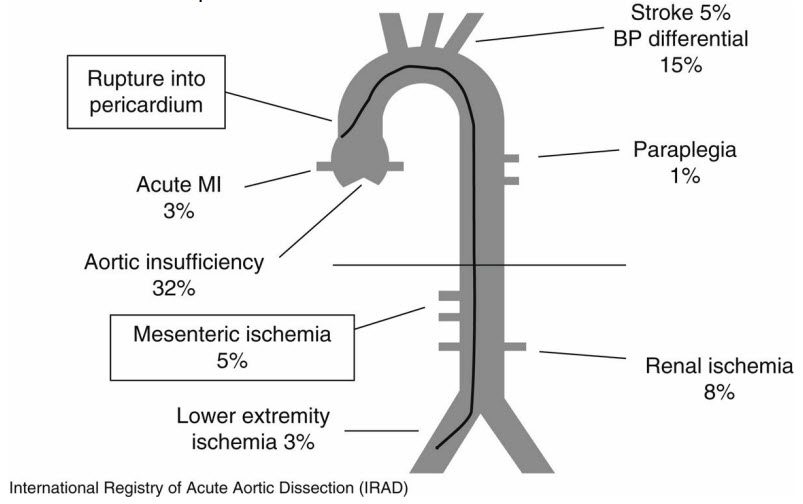
A high index of suspicion for aortic dissection is required. On examination, an upper extremity pulse deficit and/or blood pressure differential should be evaluated, and so bilateral blood pressure should be measured. Imaging modalities to confirm the diagnosis include computed tomography angiography, magnetic resonance imaging angiography, transesophageal echocardiography, and aortography. While all modalities have >95% sensitivity and specificity, contemporary computed tomography angiography is reported to have a near 100% sensitivity and 98% specificity.
References:
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897-903.
- Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: systematic review and meta-analysis. Arch Intern Med. 2006;166(13):1350-1356.