Question 1#
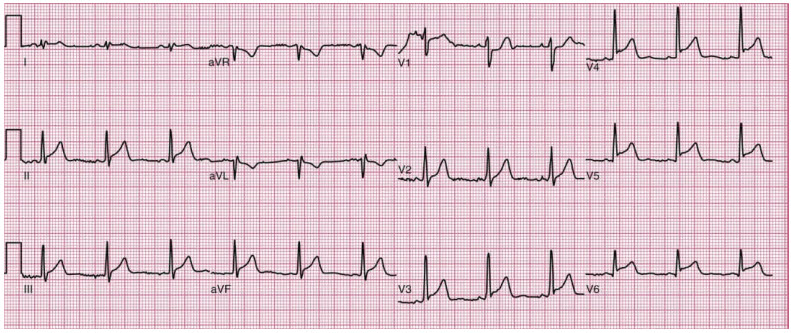
A 35-year-old male with no significant past medical history presents to the Emergency Department with one day of worsening chest pain. The chest pain was abrupt in onset, is described as “sharp” in nature, and worsens with inspiration. It is primarily centered in the center of his chest but occasionally radiates to the left upper back. He feels that the pain worsens when he lays down. Vital signs are unremarkable including equal bilateral upper extremity blood pressures and radial pulses. On physical examination, he is febrile to 38.2°C. A triphasic “scratching” sound in time with the cardiac cycle is auscultated at the left lower sternal border. Initial laboratory studies show a negative troponin T and mild elevations in white blood cell count and the C-reactive protein. His ECG is shown below:
Which of the following is the most appropriate next step:
A. Heparin bolus and dripB. High-dose aspirin and colchicine
C. Corticosteroids
D. Computed tomography angiography of the chest
E. Coronary angiography
Correct Answer is B
Comment:
Correct Answer: B
This patient’s presentation is consistent with acute pericarditis. The majority of cases of acute pericarditis in developed countries are either due to viral or idiopathic causes. However, in developing nations, tuberculosis is a leading cause of pericarditis. Typical symptoms include acute onset, severe, and often sharp chest pain that is usually retrosternal, but occasionally in the left chest. The classic pattern of pericarditis pain is radiation to the trapezius ridge in the back. The pain in pericarditis is often pleuritic in nature. Additionally, it can be positional, with worsening pain with reclining and palliation with leaning forward. A low-grade fever and sinus tachycardia may be present. On physical examination a pericardial friction rub may be present and is classically heard as a triphasic scratching sound in the precordium, best heard with the patient leaning forward. However, there may be only monophasic or biphasic rub. Muffled heart sounds or elevation of the jugular venous pressure should raise immediate suspicion for a large pericardial effusion and possible tamponade physiology.
Diagnosis of acute pericarditis is a clinical decision made based on having two or more of the following: chest pain; pericardial friction rub; ECG changes with typical concave ST segment elevation spanning multiple coronary territories and/or PR depression; pericardial effusion. In addition, other morbid conditions such as acute myocardial infarction, aortic dissection, and pulmonary embolism should be considered in the differential diagnosis and excluded by appropriate clinical judgment or targeted testing. This patient has three out of four of the listed criteria and several signs and symptoms consistent with acute pericarditis.
First line treatment of the first episode of acute pericarditis thought to be secondary to viral or idiopathic causes consists of high-dose NSAIDs and weight-based colchicine dosing. The usual NSAID regimen consists of aspirin 750 to 1,000 mg every 8 hours or ibuprofen 600 to 800 mg every 8 hours for 1 to 2 weeks, followed by tapering to discontinuation over 2 to 3 weeks. Colchicine (0.5-0.6 mg every 12 hours for patients weighing >70 kg, or 0.5-0.6 mg once daily for patients weighing <70 kg) should be continued for 3 months, and then discontinued without tapering. The use of colchicine improves response to NSAID and reduces the risk of recurrent pericarditis by half. The clinical history and ECG with concave ST-segment elevations spanning multiple coronary territories are highly suggestive of acute pericarditis, and unlikely to reflect acute coronary syndrome. Therefore, initiation of heparin in this patient is not the best next step, especially as there is a theoretical risk of hemorrhagic conversion in the setting of acute pericarditis. Corticosteroids are not the first line therapy for acute pericarditis (viral or idiopathic) unless the patient cannot tolerate NSAIDs or colchicine, or if there is another indication for corticosteroids, such as an autoimmune pericarditis. Imaging studies such as CTA and coronary angiography are not as necessary at this time because acute coronary syndrome and aortic dissection are less likely given the clinical picture of pericarditis, negative troponin, ECG, and equal bilateral blood pressures.
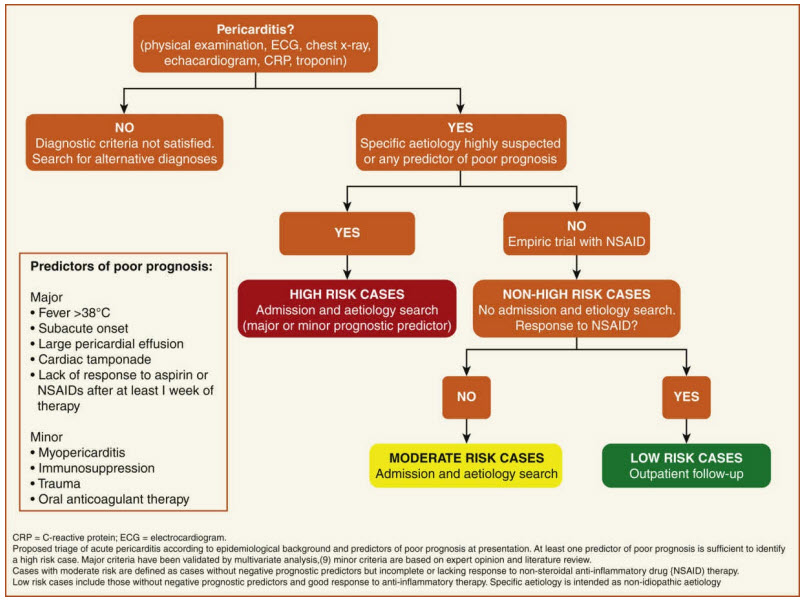
(Figure from Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC). Eur Heart J. 2015;36:2921.)
References:
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC). Eur Heart J. 2015;36:2921.
- LeWinter MM. Clinical practice. Acute pericarditis. N Engl J Med. 2014;371:2410.
- Imazio M, Gaita F. Diagnosis and treatment of pericarditis. Heart. 2015;101:1159.
- Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA. 2015;314:1498.
- Dudzinski DM, Mak GS, Hung JW. Pericardial diseases. Curr Probl Cardiol. 2012;37:75.