Question 5#
A 67-year-old male with history of former smoking, hypertension, diabetes, and stage III small cell lung cancer (on chemotherapy) presents to the Emergency Department with 3 days of progressive shortness of breath and an episode of syncope.
Vital signs show:
- temperature of 36.6°C
- regular heart rate of 130 beats per minute
- room air oxygen saturation of 94%
Blood pressure at rest is 96/54 mm Hg at end inspiration and drops to 82/50 mm Hg with inspiration. Physical examination reveals a pale cachectic and uncomfortable appearing male with cool extremities, muffled heart sounds, and jugular venous pressure of 14 cm H2O.
Laboratory studies are remarkable for:
- creatinine 2.5 mg/dL (baseline 1.0)
- hemoglobin 7.5 g/dL (baseline 8.0)
- platelets 120,000/µL
- white blood cell count 13,000/µL
- CRP 4.2 mg/L
- troponin T 0.1 ng/dL
- NT proBNP 8,000 pg/mL (no known baseline)
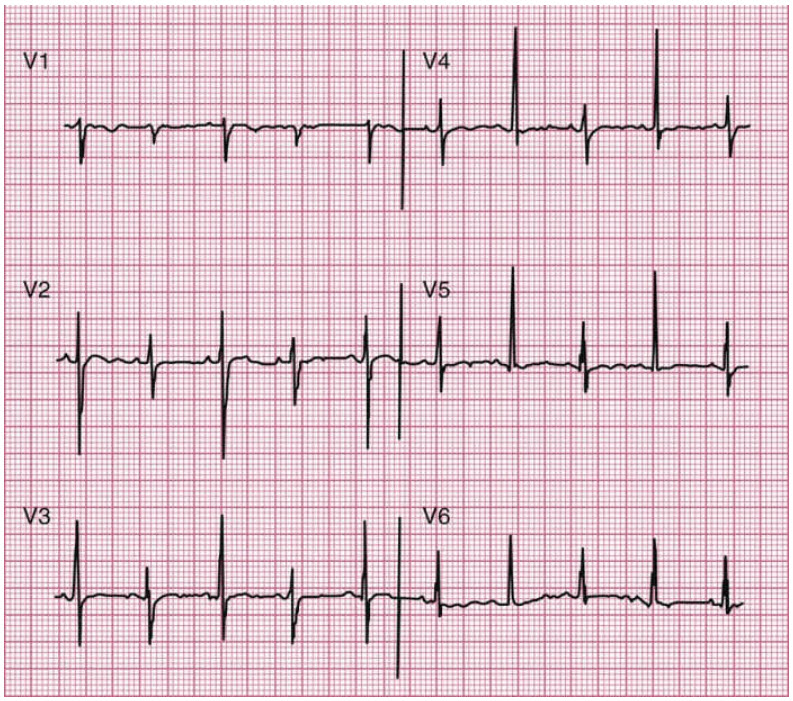
Precordial leads from his ECG are shown in the figure that follows:
What is the appropriate next diagnostic step?
A. Limited echocardiogramB. CTA of the chest and abdomen (arterial phase)
C. Coronary angiography
D. CT chest pulmonary embolism protocol
E. Cardiac MRI
Correct Answer is A
Comment:
Correct Answer: A
This patient is presenting with evolving cardiogenic shock (hypotension, cool extremities, syncope, and evidence of organ dysfunction with acute kidney injury), likely due to pericardial tamponade. The next appropriate step is emergent limited echocardiography, to accompany emergent pericardiocentesis. Pericardial tamponade is a life-threatening emergency in which pressure in the pericardial space rises due to a variety of possible reasons, leading to compression of the heart, ultimately impairing cardiac output and leading to shock or death. Causes of pericardial tamponade are similar to those that cause pericardial effusions and are listed in the table that follows. In the case of this patient, his history of progressive lung cancer makes a malignant effusion most likely.
Pulsus paradoxus is an important physical finding in cardiac tamponade. Pulsus paradoxus refers to an abnormally large reduction in both the stroke volume and the systemic blood pressure with inspiration, which in pericardial tamponade is due to the extrinsic constraint on cardiac chamber expansion leading to enhanced ventricular interdependence. Transthoracic echocardiogram is the imaging modality of choice in diagnosing and guiding management of cardiac tamponade. Cardiac CT and MRI can be utilized to better understand the pericardium and help understand the cause of tamponade, but are rarely indicated in the acute setting.
Here, the patient is in cardiogenic shock and needs urgent imaging of the pericardium with a limited echocardiogram to guide treatment. Cardiac MRI, CTA chest, and CT chest would not add to the immediate management of this patient, as aortic dissection and pulmonary embolism are less likely based on clinical presentation. Coronary angiography is not warranted because there is no evidence of acute coronary syndrome. The troponin elevation, in this case, is explained by damage from cardiogenic shock rather than acute plaque rupture.
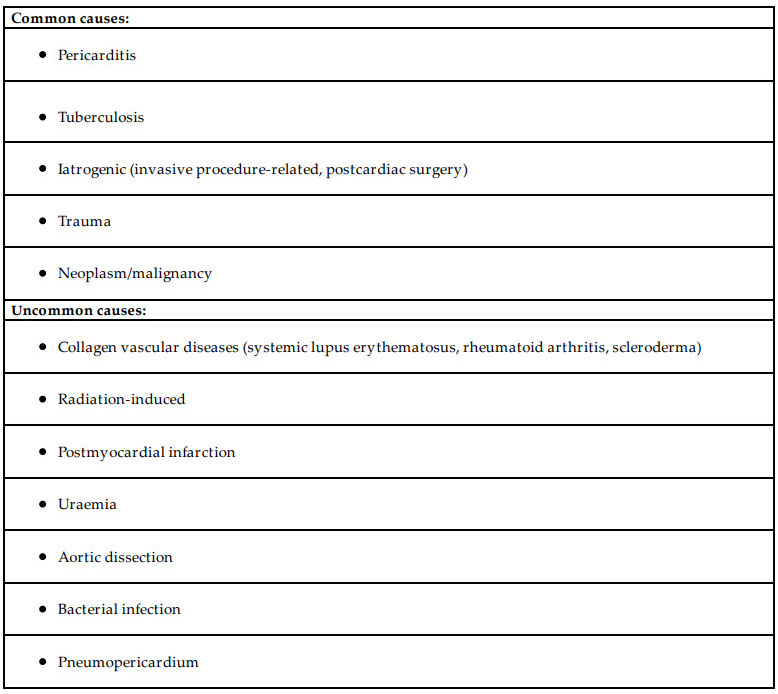
Causes of cardiac tamponade:
Table from Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC). Eur Heart J. 2015;36:2921.
References:
- Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier/Saunders; 2018.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC). Eur Heart J. 2015;36:2921.