Question 2#
A 75-year-old female with prior history of hypertension and hyperlipidemia presents with acute onset chest pain and dyspnea for last 4 hours ago. Physical examination revealed bilateral rales, cool extremities, and diaphoresis. She had no murmurs on auscultation. ECG revealed 1.5-mm ST segment elevations throughout the precordial leads. High-sensitivity troponin was elevated at 100 ng/L. Left coronary angiogram reveals nonobstructive coronary disease and ventriculography shows apical ballooning with sparing of base as well as globally reduced ejection fraction.
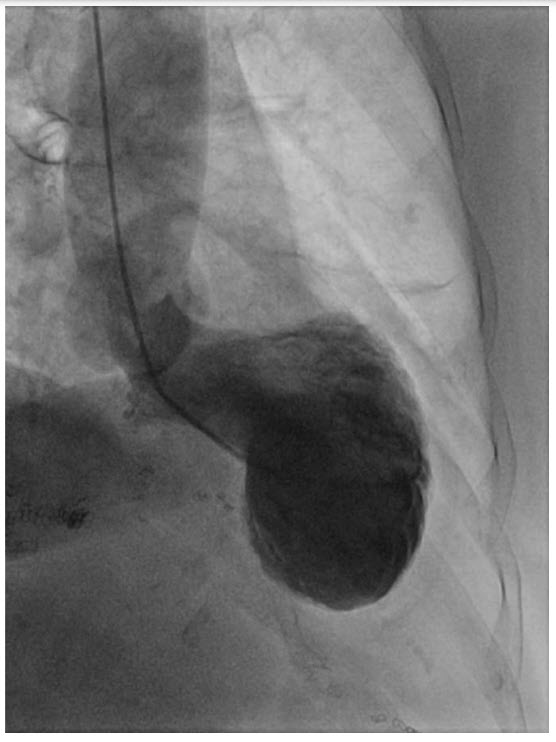
Left ventriculography on cardiac catheterization.
On arrival to the ICU she has bibasilar rales with oxygen requirement of 6 L/min via nasal cannula. Blood pressure is 95/48 mm Hg and HR is 122 beats per minute.
Which of the following medications should be avoided at this stage?
A. DiureticsB. Beta blockers
C. Nitrates
D. Levosimendan
Correct Answer is B
Comment:
Correct Answer: B
Patients with Takotsubo cardiomyopathy often have a clinical presentation that is similar to those patients presenting with acute coronary syndrome. The wall motion abnormalities seen in Takotsubo cardiomyopathy extend beyond a single vascular territory, but multivessel coronary lesions must be excluded. Diagnostic modality of choice is coronary angiography. When obstructive coronary artery disease is seen in one vessel, but the wall motion abnormalities extend beyond one vascular territory, the diagnosis of Takotsubo cardiomyopathy may be suggested. The most classic phenotype of Takotsubo cardiomyopathy is the apical ballooning with basilar sparing, seen on left ventricular catheterization or on transthoracic echocardiography. Other morphologies include midventricular, biventricular, and an “inverted” form with basal hypokinesis. The underlying pathophysiology is thought to be related to catecholamine surge resulting in myocardial myocyte dysfunction. Takotsubo cardiomyopathy is more likely to affect women than men and often occurs in postmenopausal women who experienced a hemodynamic, physical, or emotional stressor. It can occur secondary to medical conditions including sepsis, subarachnoid hemorrhage, and pheochromocytoma. Mortality is similar to that of STEMI in the acute phase for hospitalized patients, 4% to 5%. Complications of Takotsubo cardiomyopathy include cardiogenic shock, severe mitral regurgitation, arrhythmias, pulmonary edema, and left ventricular outflow tract obstruction (particularly in patients with preexisting left ventricular upper septal hypertrophy).
Studies have reported increased mortality in Takotsubo cardiomyopathy with catecholamines. However, a calcium sensitizer called levosimendan may theoretically be used in place of inotropes and vasopressors, though this medication is not available in the United States. ACE inhibitors may help with recovery of cardiac function but should be avoided in the early phase of cardiogenic shock. Beta blockers have not shown benefit in Takotsubo cardiomyopathy and are contraindicated in cardiogenic shock or decompensated heart failure. Management is guided by standard heart failure measures, including afterload reduction and diuresis.
References:
- Pelliccia F. Pathophysiology of takotsubo syndrome. Circulation. 2017;135:2426-2441.
- Santoro F, Ieva R, Ferraretti A, et al. Safety and feasibility of levosimendan administration in takotsubo cardiomyopathy: a case series. Cardiovasc Ther. 2013;31:e133-e137.