Question 1#
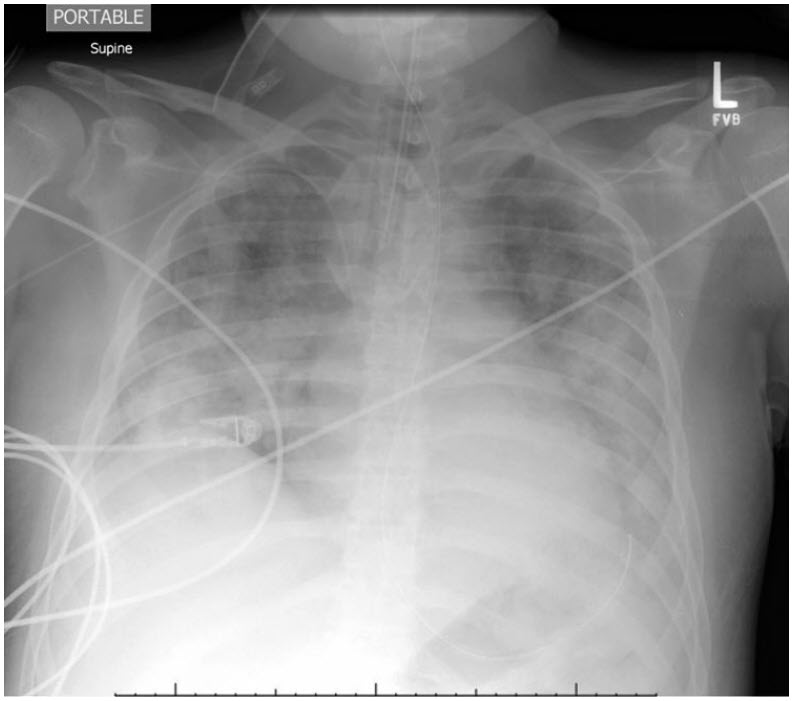
A 40-year-old previously healthy 90-kg man (ideal body weight of 80 kg) walks into the Emergency Department (ED) complaining of 5 days of myalgias, fevers, rhinorrhea, and dry cough. Over the last day, he has become short of breath walking across the room. In the ED, he is febrile, hypotensive requiring vasopressors, with a respiratory rate of 30 and SpO2 88% on a non-rebreather face mask. He receives 30 mL/kg crystalloid and develops worsening work of breathing requiring endotracheal intubation 2 hours after arrival in ED. Endotracheal tube placement is confirmed by end-tidal CO2 and bilateral breath sounds. His SpO2 nadir is 75% but despite 5 minutes of bagging his SpO2 remains in the mid-80s. His chest X-ray is shown below:
Which of the following statements is true?
A. Following ARDSnet ventilation at 6 mL/kg, if his Plateau airway pressure is 35 cm H2O on PEEP of 14, his goal tidal volume should be 480 mLB. Given hypotension and severe respiratory failure, a PA catheter should be placed to optimize cardiac filling pressures and improve his chances of survival
C. A strategy of doing a recruitment maneuver followed by lowering PEEP until lung compliance is maximal will improve his chances of survival
D. Inhaled nitric oxide is likely to improve his PaO2 /FiO2 ratio
E. Proning this early in ARDS has not been shown to favorably affect survival
Correct Answer is D
Comment:
Correct Answer: D
The ARMA trial randomly assigned 861 patients with ARDS to low tidal volume ventilation (6 mL/kg predicted body weight) or 12 mL/kg PBW. The 6 mL/kg group had a lower risk of 28-day mortality (RR 0.74, CI 0.61-0.88). A subsequent meta-analysis found similar results. Importantly, the ARMA protocol targeted both a tidal volume of 6 mL/kg and plateau pressure <30 cm H2O. Because this patient had a plateau pressure of 35 cm H2O on 6 mL/kg PBW, the protocol would advise further reductions in tidal volume to a minimum of 4 mL/kg PBW.
The fluid and catheter treatment trial randomized 1,000 patients with acute lung injury to management with a central venous catheter or PA catheter, finding no difference in 60-day survival. Furthermore, there was no evident benefit of the PAC in the duration of shock, ventilator-free days, fluid balance, or measures of lung or kidney function. The PAC group had significantly more catheter-related complications, mostly arrhythmias (and some cases of conduction block).
Lungs afflicted with diffuse injury are edematous and have poor compliance. The multicenter ART trial randomized 1,010 patients with moderate to severe ARDS to low tidal volume ventilation using a low-PEEP FIO2 /PEEP grid (as in ARMA) or a recruitment maneuver/decremental PEEP strategy: following neuromuscular blockade and using pressure control ventilation, PEEP raised from 25 to 35 and then 45 cm H2O for 2 minutes, and then dropped to 23 cm H2O and reduced 3 cm H2O at a time down to a minimum of 11 cm H2O with static compliance measured at each step, settling on 2 cm H2O above the PEEP yielding the highest compliance. The recruitment maneuver group suffered a higher 28-day mortality (HR 1.20, CI 1.01-1.42), reduced ventilator-free days, and increased risk of barotrauma including pneumothorax-requiring drainage.
Inhaled nitric oxide has long-been known to improve oxygenation by selectively improving blood flow to aerated regions of lungs, improving ventilation-perfusion matching, which is frequently impaired during critical illness. Indeed, in a meta-analysis of 12 randomized trials, iNO was found to increase the PaO2 /FiO2 ratio. However, this same meta-analysis showed that patients receiving iNO had a trend toward higher mortality (RR 1.10, CI 0.94-1.30) and significantly increased renal dysfunction (RR 1.50, CI 1.11-2.02).
The PROSEVA study randomized 455 patients with severe ARDS and intubated <36 hours to undergo prone-positioning of at least 16 hours daily or be left in the supine position. Prone positioning was associated with a dramatic improvement in 28-day mortality (HR 0.39, CI 0.25-0.63). Notably, prone positioning is occasionally utilized during the management of refractory hypoxemia in patients who have been intubated for many days. The PROSEVA study, by contrast, proned patients early in the course of their illness. The mechanism of benefit is not known with certainty, but speculated to be related to a reduction in ventilator injury owing to more even distribution of strain (because the proned ARDS lung has more uniform mechanical characteristics than the supine ARDS lung.)
References:
- The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301-1308.
- Petrucci N, De Feo C. Lung protective ventilation strategy for the acute respiratory distress syndrome. Cochrane Database Syst Rev. 2013; (2):CD003844. doi:10.1002/14651858.CD003844.pub4.
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wheeler AP, Bernard GR, Thompson BT, et al. Pulmonary-Artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354:2213- 2224.
- Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura ÉA, Laranjeira LN, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335-1345.
- Adhikari NK, Burns KE, Friedrich JO, et al. Effect of nitric oxide on oxygenation and mortality in acute lung injury: systematic review and meta-analysis. BMJ. 2007;334:779.
- Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159-2168.
- Gattinoni L. Taccone P. Carlesso E. Marini JJ. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med. 2013;188:1286-1293.