Question 4#
A 70-year-old male with a history of chronic obstructive pulmonary disease (COPD), requiring prior intubation, and active tobacco use presents to the emergency department with shortness of breath. He states that over the last 24 hours, he has had increasing difficulty breathing. He denies fevers or chills at home and is not aware of any sick contacts. His initial vitals are:
- temperature of 99.4 F
- heart rate 90/min
- blood pressure 130/80 mm Hg
- respiratory rate 22/min
- SpO2 95%
On examination, he appears to have a mild increase in work of breathing. He is noted to have scattered wheezing throughout both lung fields. He is started on albuterol nebulizers and IV steroids. Three hours into his emergency room stay you are called to the bedside as the patient appears to be in more distress. His vitals demonstrate:
- temperature of 99.8
- HR 125
- BP 120/70 with an RR of 35
- SpO2 90%
On examination, the patient is using accessory muscles, and his lung examination is notable for poor air movement with no wheezing. An arterial blood gas is performed:
- pH 7.28
- PCO2 50
- PaO2 65
A chest x-ray is performed and demonstrates hyperinflation of both lung fields with no infiltrate. He is intubated for hypoxemic respiratory failure and is subsequently paralyzed with a neuromuscular blocker secondary to ventilator dyssynchrony. He arrives to the ICU ventilated, with an FiO2 of 0.8, PEEP 10, RR 30, and TV 420 mL/kg (the patient weighs 70 kg). His arterial blood gas demonstrates a pH 7.29/PCO2 50/PaO2 200. His blood pressure upon arrival to the ICU is 80/50 mm Hg.
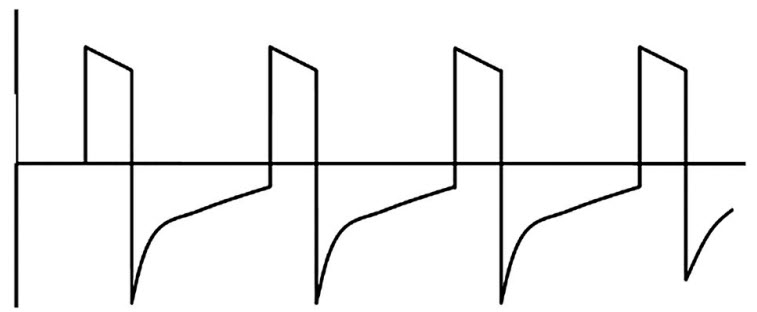
His flow/time wave form is noted in the following figure:
What would be the next step in management?
A. Increase his tidal volumesB. Increase his PEEP from 10 to 15
C. Decrease the respiratory rate
D. Increase the inspiratory time
Correct Answer is C
Comment:
Correct Answer: C
The figure above demonstrates air trapping or “auto-PEEP” as the exhalation wave form fails to reach zero before the next breath is taken. Auto-PEEP can cause decreased venous return which leads to a decrease in cardiac output and results in hypotension which was seen in this patient. To address air trapping, the key is to increase the expiratory time. Decreasing the respiratory rate is an affective way to achieve a longer exhalation period. Another way to enhance the expiratory time is to change the inspiration:expiratory ratio or the I:E time. This can be accomplished by increasing the inspiratory flow rate thus decreasing the inspiratory time. Increasing the patient’s tidal volume could enhance the minute ventilation; however, it would not address the dynamic hyperinflation. Finally increasing PEEP can have variable effects on the intrathoracic pressure depending on the degree of expiratory flow limitation but is unlikely to decrease the auto-PEEP.
Reference:
- Ward N, Dushay K. Clinical concise review: mechanical ventilation of patients with chronic obstructive pulmonary disease. Crit Care Med. 2008;36(5):1614-1619.