Question 2#
A 17-year-old college student is admitted to the hospital after sustaining a traumatic hit to the head during football practice, resulting in subdural hemorrhage. Upon arrival, his Glasgow Coma Scale is 4. He is started on hypertonic saline and undergoes emergent neurosurgical intervention. His exam remains unchanged overnight, but during morning rounds, the nurse reports that his urine output increased to over 300 mL/h.
Laboratory studies obtained show:
- serum sodium 167 mEq/L
- specific gravity 1.013
- random urine sodium 55 mEq/L (mmol/L)
- random urine creatinine 51 mg/dL
- urine osmolality 199 mOsm/kg H2O
- serum osmolality 338 mOsm/kg H2O
Which is the MOST likely cause of his increased urine output?
A. Syndrome of inappropriate antidiuretic hormone secretion (SIADH)B. Central diabetes insipidus (DI)
C. Cerebral salt wasting (CSW) syndrome
D. Nephrogenic diabetes insipidus (NDI)
E. Osmotic diuresis
Correct Answer is B
Comment:
Correct Answer: B
Central DI occurs in the setting of inadequate production of ADH. Normally, ADH is secreted by the posterior pituitary gland. However, in patients who sustained traumatic brain injury, a decrease or cessation of ADH production can occur, thereby decreasing reabsorption of water leading to hypernatremia. In otherwise healthy patients, the lack of ADH will cause increased thirst and lead to polydipsia. These symptoms might not be apparent in a critically ill patient.
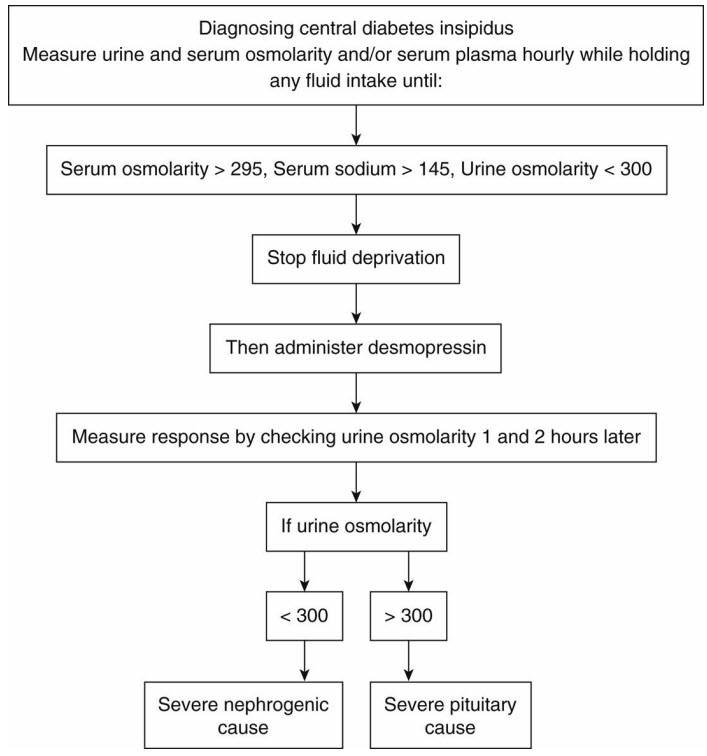
Water deprivation test and administration of desmopressin, as depicted in the flowchart below, may be used to confirm the diagnosis. However, the test is relatively contraindicated in hypovolemic and hypernatremic patients due to risk of exacerbating these. Further testing is not needed in our patient, since the clinical presentation and laboratory studies are consistent with central DI. Diagnostic evaluation for suspected DI includes serum sodium, serum, and urine osmolality, which are expected to show hypernatremia with decreased urine osmolality <600 mOsm/kg and serum osmolality of >295 mOsm/kg. In patients with central DI, the urine osmolality is expected to increase by >100% after administration of desmopressin.
References
- Robertson GL. Diabetes insipidus. Endocrinol Metab Clin North Am. 1995;24(3):549-572.
- Makaryus AN, McFarlane AI. Diabetes insipidus: diagnosis and treatment of a complex disease. Clev Clin J Med. 2006;73(1):65-71.