Question 3#
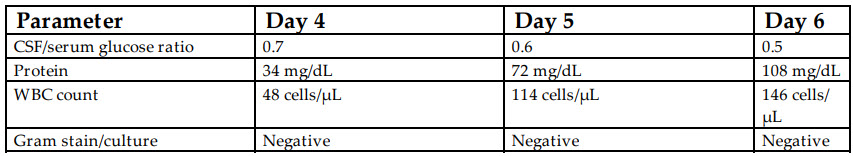
A 42-year-old woman is admitted to the neurological ICU after presenting with worsening mentation and the finding of a new intracranial mass on MRI. She is intubated for airway protection and has a external ventricular drain (EVD) placed for management of obstructive hydrocephalus. On ICU day 1, she is afebrile and hemodynamically stable. Over the next 3 days, she has a low-grade fever (99.5-100°F), and on ICU day 5, she has a fever of 100.8°F. CSF drawn from the EVD on day 4 to day 6 shows the following results:
Based on the CSF results, what is the most appropriate next step in management?
A. Repeat the MRI to inform further management of the intracranial disease processB. Defer any intervention unless CSF cultures show any growth
C. Start empiric intraventricular vancomycin and cefepime
D. Start empiric intravenous (IV) vancomycin and cefepime
Correct Answer is D
Comment:
Correct Answer: D
The patient has evidence of a ventriculostomy-related infection and should be treated with broad-spectrum empiric IV antimicrobial therapy. Healthcare-associated ventriculitis and meningitis (HAVM) accounts for a significant proportion of CNS infections seen in institutions with neurosurgical facilities. However, diagnosis of HAVM based on CSF findings can be challenging especially in the setting of a known neurological disease process or recent neurosurgical intervention. The microbiology of healthcare-associated meningitis differs fundamentally from community-acquired meningitis. The most common pathogens in the healthcare setting are Staphylococcus aureus, Staphylococcus epidermidis, Propionibacterium acnes, and Enterobacteriaceae (including Serratia in the postoperative setting).
CSF drain–related ventriculitis has an incidence of 8% to 9% per patient or per EVD placement. However, the diagnosis is often difficult to establish in critically ill patients where clinical examination and symptomatic assessment are limited. Clinical symptoms which should raise suspicion for HAVM include CSF pleocytosis, hypoglychorrachia, increasing CSF protein and/or cell counts, and positive CSF gram stain or cultures. In general, an isolated positive CSF gram stain and/or culture is not considered diagnostic for HAVM, and contamination or colonization is more likely. Given the indolent nature of some pathogens common in this setting (eg Staphylococcus epidermidis, Propionibacterium acnes), CSF cultures may take several days to show growth, which may mislead clinicians and delay the diagnosis of HAVM. Lozier’s classification is often used to support treatment decisions for HAVM:
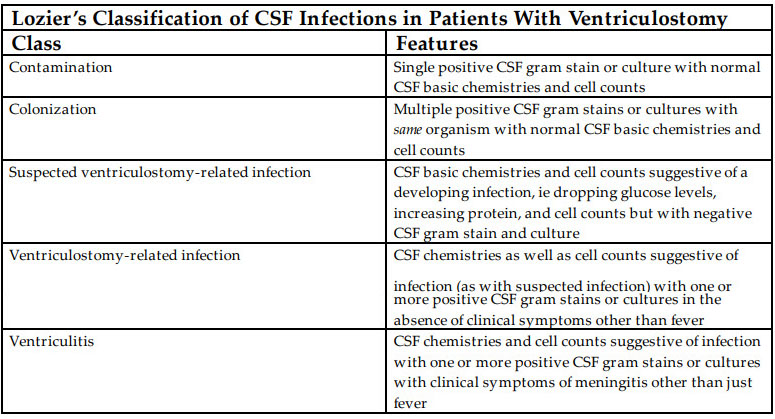
Empiric therapy for HAVM is directed at the common pathogens and often consists of IV vancomycin and a third or fourth generation cephalosporin to provide Pseudomonas coverage. Intrathecal therapy is usually reserved for poor response to IV therapy or when pathogens are known to have high minimum inhibitory concentrations (MICs), which are not likely to be attainable via the IV route. In a penicillin- or cephalosporin-allergic patient, aztreonam may be used instead of a cephalosporin.
References:
- Lozier AP, Sciacca RR, Romagnoli MF, Connolly ES. Ventriculostomyrelated infections: a critical review of the literature. Neurosurgery. 2008;62(suppl 2):688-700.
- Tunkel AR, Hasbun R, Bhimraj A, et al. 2017 Infectious diseases Society of America’s clinical practice guidelines for healthcare-associated ventriculitis and meningitis. Clin Infect Dis. 2017. doi:10.1093/cid/ciw861.
- O’Horo JC, Sampathkumar P. Infections in neurocritical care. Neurocrit Care. 2017;27:458-467.