Question 1#
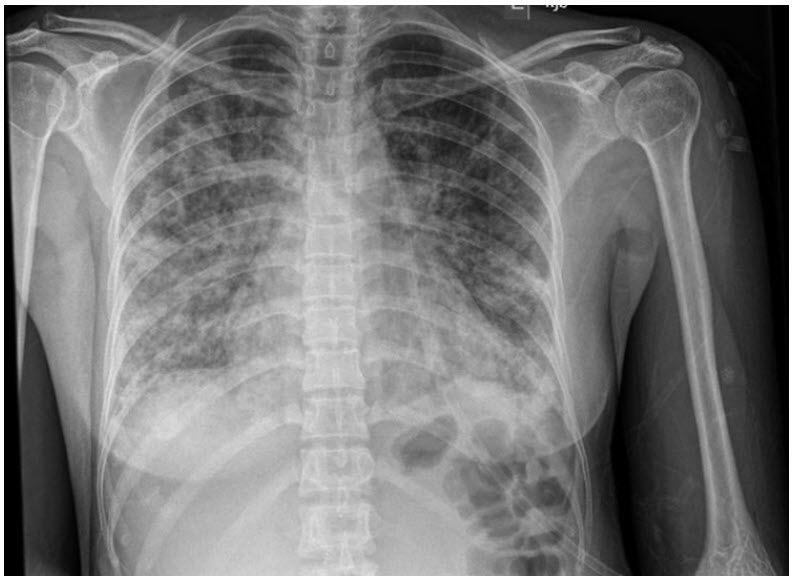
A 52-year-old woman diagnosed with granulomatosis with polyangiitis (Wegener’s) 3 months ago and treated with cyclophosphamide and prednisone (40 mg daily) presents to ED due to shortness of breath and dry cough. Last time she noted bloodtinged sputum was more than 2 months ago. Her vitals on arrival are notable for temperature of 39.2°C, heart rate 110 beats/min, blood pressure 104/54, respiratory rate 25 breaths/min, and oxygen saturation 86% on room air. Chest x-ray reveals bilateral infiltrates and cystic-appearing round opacities (fig below):
She is placed on high flow nasal cannula at 55 L/min and FiO2 of 0.8, but her respiratory distress continues to worsen, and she requires endotracheal intubation. Her labs are notable for Arterial blood gas:
- pH 7.48
- pCO2 23
- pO2 58 (before intubation)
Lactate dehydrogenase (LDH): 664 (normal: 110-210 U/L)
Which of the following treatment regimens would MOST likely improve her condition?
A. Ceftriaxone and azithromycinB. Trimethoprim/sulfamethoxazole
C. Oseltamivir
D. Isoniazid
Correct Answer is B
Comment:
Correct Answer: B
Patient has clinical symptoms and laboratory and radiographic signs consistent with pneumocystis jirovecii pneumonia (PJP), an opportunistic infection typically affecting immunocompromised hosts. These may include patients with acquired immune deficiency syndrome (AIDS), those with malignancies, stem cell and solid organ transplant recipients, and patients receiving high-dose corticosteroids and other immunosuppressants. PJP classically presents with fever, dry cough, and hypoxemic respiratory failure with exertional oxygen desaturations. Positive PJP PCR or silver stain from induced sputum or bronchoalveolar lavage (BAL) samples are confirmatory. LDH elevation is common, particularly in HIV-positive patients in whom the sensitivity is reported to be 100%; however, sensitivity is lower (∼60%) in HIV-negative individuals. Radiographic findings include bilateral patchy infiltrates with cysticappearing opacities on chest x-rays (as seen in the above chest x-ray). On high-resolution CT scans, the most common findings are ground glass opacities with cysts that are seen in approximately one third of patients. First-line treatment is intravenous trimethoprim/sulfamethoxazole (Bactrim) which should be continued for at least 7 to 10 days or until clinical improvement is seen, when transition to oral antibiotics is considered. Total duration of therapy is typically 3 weeks. PJP prophylaxis should be initiated in patients with CD4 count less than 200 cells/mm3 and those receiving high-dose steroids (>20 mg/d) for more than one month, particularly if the patient is receiving additional cytotoxic agents, as in this clinical vignette.
References:
- Kanne JP, Yandow DR, Meyer CA. Pneumocystis jiroveci pneumonia: high-resolution CT findings in patients with and without HIV infection. Am J Roentgenol. 2012;198(6):555-561.
- Limper AH, Knox KS, Sarosi GA. An Official American Thoracic Society Statement: treatment of fungal infections in adult pulmonary and critical care patients. Am J Resp Crit Care Med. 2011;183(1):96-128.
- Smith DE, Forbes A, Davies S, Barton SE, Gazzard BG. Diagnosis of Pneumocystis carinii pneumonia in HIV antibody positive patients by simple outpatient assessments. Thorax. 1992;47(12):1005-1009.
- Vogel MN, Weissgerber P, Goeppert B, et al. Accuracy of serum LDH elevation for the diagnosis of Pneumocystis jiroveci pneumonia. Swiss Med Wkly. 2011;141:w13184.
- Wieruszewski PM, Barreto JN, Frazee E, et al. Early corticosteroids for pneumocystis pneumonia in adults without HIV are not associated with better outcome. Chest. 2018;154(3):636-644.